PARTICIPATE
CONNECT
MAKE A DIFFERENCE
JOIN US
Medical Aid-in-Dying (“MAiD”) is medical assistance provided to a terminally ill patient who has decisional capacity enabling them to self-administer prescribed medications, following an explicit written request in order to end their life in a manner that is safe, certain, and painless.
The prerogative to refuse life-sustaining and life-prolonging interventions via an advance directive is an established legal, ethical, and moral right. Controversy remains as to whether patients with dementia have an equivocal right to refuse assisted feeding at the end of life through an advance directive made when the patient had decision-making capacity.
In 2022, Assemblymember Richard N. Gottfried retired. The New York State Bar Association's Health Law Session held a full-day program on November 3 to honor his impact on healthcare in New York. The program focused on his contributions to healthcare access, civil liberties, decision making, and oversight. Robert N. Swidler interviewed Gottfried at the end of the program.
The Joint Commission, which accredits hospitals in the United States, recently eliminated the performance standard for clinical ethics services. This decision has raised concerns among members of the New York's Empire State Bioethics Consortium and other bioethics leaders across the country.
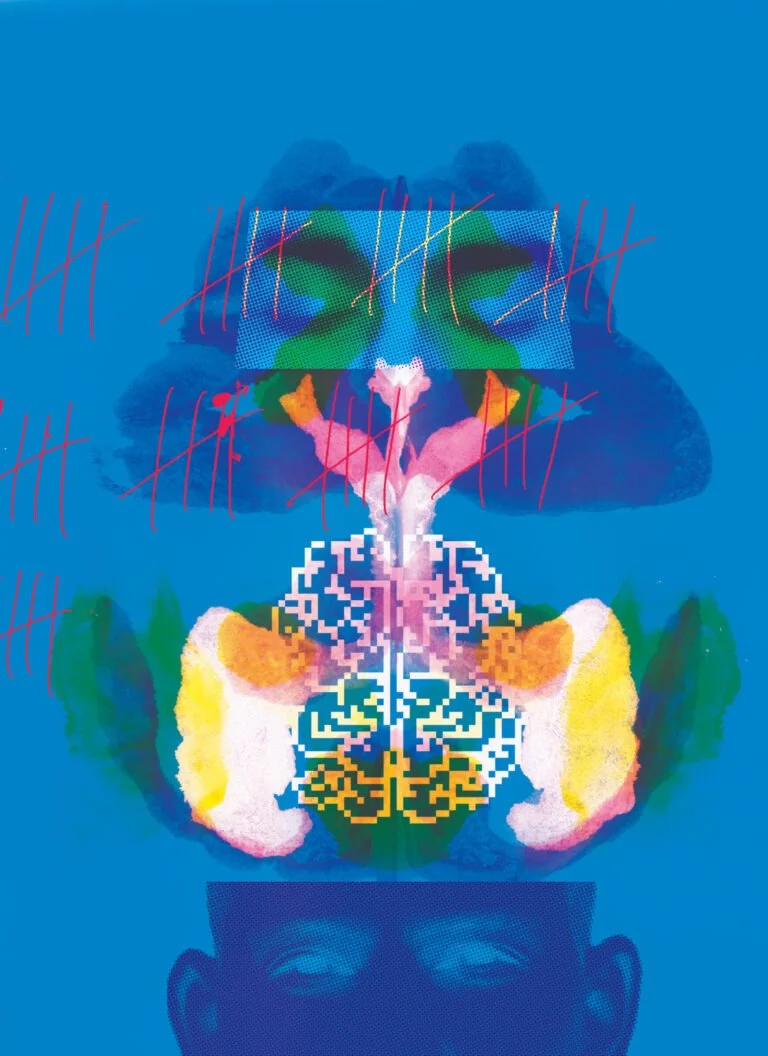
An Arkansas man’s unprecedented recovery of consciousness, and his recent death, demonstrate why progress in neuroscience must be matched by new standards of care for patients as well as attention to their civil rights.
Moral dilemmas have arisen concerning whether physicians and other providers should treat patients who have declined COVID vaccination and are now sick with this disease. Several ethicists have argued that clinicians have obligations to treat such patients, yet providing care to these patients has distressed clinicians, who have at times declined to do so. Critical questions thus emerge regarding how best to proceed.
By considering the history of bioethics and international humanitarian law, Joseph J. Fins contends that bioethics as an academic and moral community should stand in solidarity with Ukraine as it defends freedom and civility.
In March 2020, ethics professionals in New York City began virtual meetings to share insights. Participants included representatives from institutions like Greater New York Hospital Association, Hastings Center, Memorial Sloan Kettering Cancer Center, Montefiore Medical Center, Mount Sinai Hospital, New York Presbyterian Columbia University & Weill Cornell Medical Centers, NYC Health & Hospitals, and others.
In the face of a relentless COVID-19 surge, hospitals nationwide grappled with unprecedented challenges of overcrowding and understaffing. Amidst the crisis, a pivotal question arose - should hospitals consider transferring inpatients to other facilities without patient or family consent?
The COVID-19 experience exposed weaknesses in New York's process of deliberative democracy in response to the pandemic. A state with a distinguished history in this interdisciplinary space was left behind with the views of important constituencies left unheard and communities unserved.










In 2023, New York State Legislature passed a bill to repeal the outdated 1987 Do-Not-Resuscitate (DNR) Law. The repeal is a technical clean-up measure because DNR orders are now governed by other laws in most cases, making the old law largely irrelevant. This change is noncontroversial and mainly affects psychiatric hospitals and units.